The Gut: A Living Garden Within
If you’ve just joined us here at The Wild Remedy, welcome.
This journal is part of an ongoing journey — my own deepening exploration of herbal medicine, the human body, and what it really means to live well in a modern world that often feels disconnected from nature, rhythm, and our own inner intelligence. Alongside my work with plants, workshops, products, and community spaces, I’m currently studying herbal medicine more formally, and again and again I’m struck by the same truth: nothing exists in isolation.
Plants, people, body systems, seasons, movement, nourishment — everything is connected.
So when the topic of the gut emerged in my studies, it felt like a natural place to pause and reflect. Digestion, immunity, mood, energy, inflammation, resilience — so many threads of health meet here. This isn’t about trends or optimisation. It’s about understanding how we are designed, how we’ve drifted away from that design, and how gently returning to it can support real, sustainable wellbeing.
There’s something quietly humbling about studying the human body the more closely you look.
The gut alone — this long, looping, intelligent system tucked into our abdomen — is enough to stop you in your tracks. Every fold, every layer, every interaction between nerve, tissue, microbe and movement feels intentional. Fearfully and wonderfully made, as the Psalmist wrote — not as poetry alone, but as lived biology.
The gut as a garden
The term gut flora has always fascinated me.
Flora comes from the Latin word for plants, and from Flora, the Roman goddess of flowers and growth. Early anatomists — many of them German and Central European — used this language because what they observed under early microscopes behaved less like animals and more like plant life: growing, fermenting, responding to nourishment and neglect.
And in many ways, the gut really is a garden.
A living ecosystem. One that must be:
fed,
tended,
rested,
moved,
and occasionally left alone.
When we nourish it well, diversity thrives. When we over-interfere, strip it back, or flood it with artificial inputs, imbalance creeps in quietly rather than dramatically.
This isn’t new knowledge.
It’s modern science slowly catching up with ancient wisdom.
Flora Roman Goddess
What the gut actually is (and why it matters)
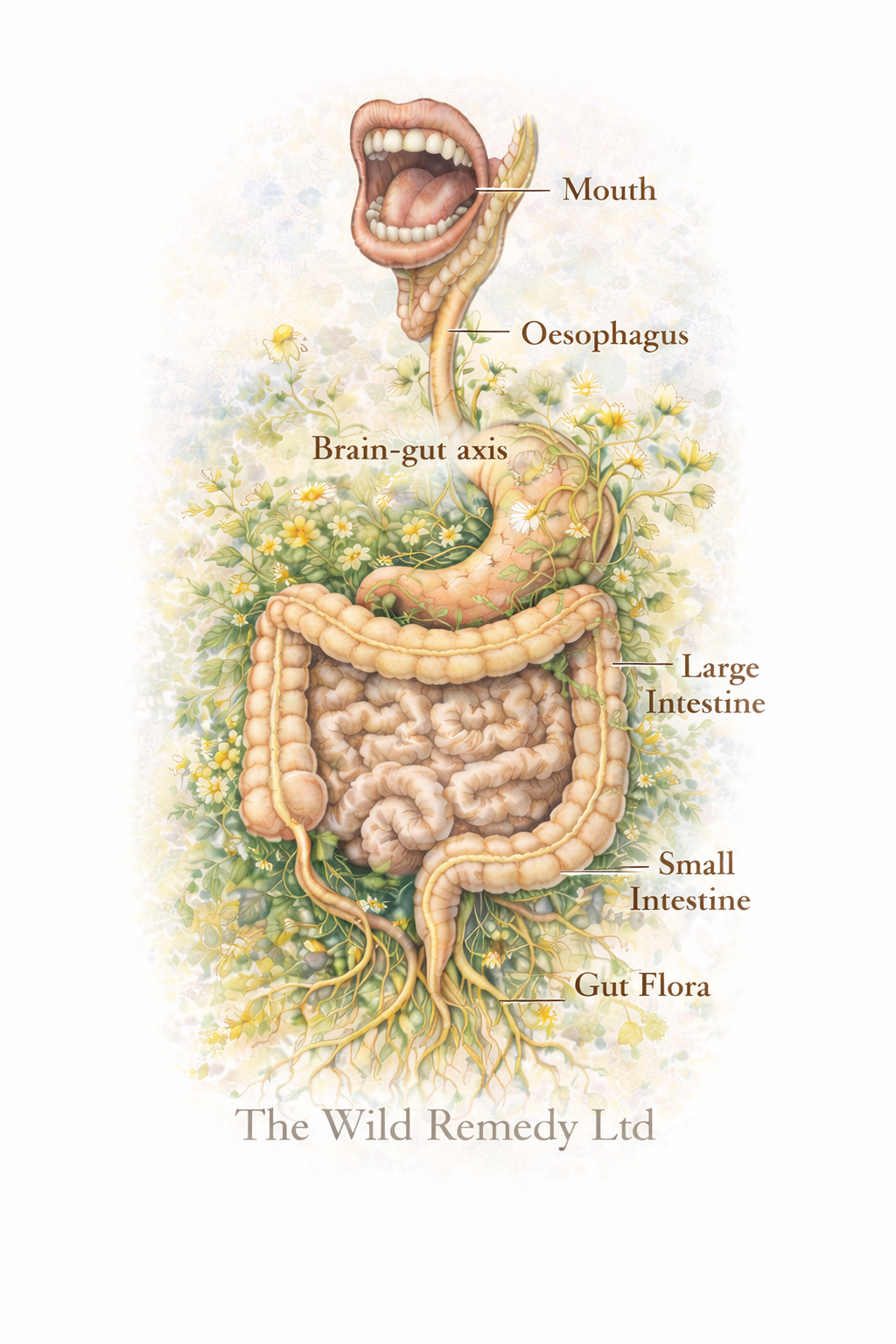
It’s easy to talk about the gut as though it were a single thing — a place, a problem, a box to tick on a health checklist. But when you really sit with it, the gut reveals itself as something far more layered and alive.
It begins at the mouth and winds its way through the body, folding and looping to fit inside us, never static, never switched off. A soft, muscular passage that senses, responds, and adapts moment by moment. It meets everything we take in from the outside world and decides — quietly, continuously — what becomes part of us and what does not.
Along its length, the gut is alive with intelligence. Nerve cells woven through its walls. Immune tissue standing watch at the boundary between inner and outer worlds. Microbial life settling where it feels supported, retreating where it does not. This is not a passive tube — it is a place of constant communication and discernment.
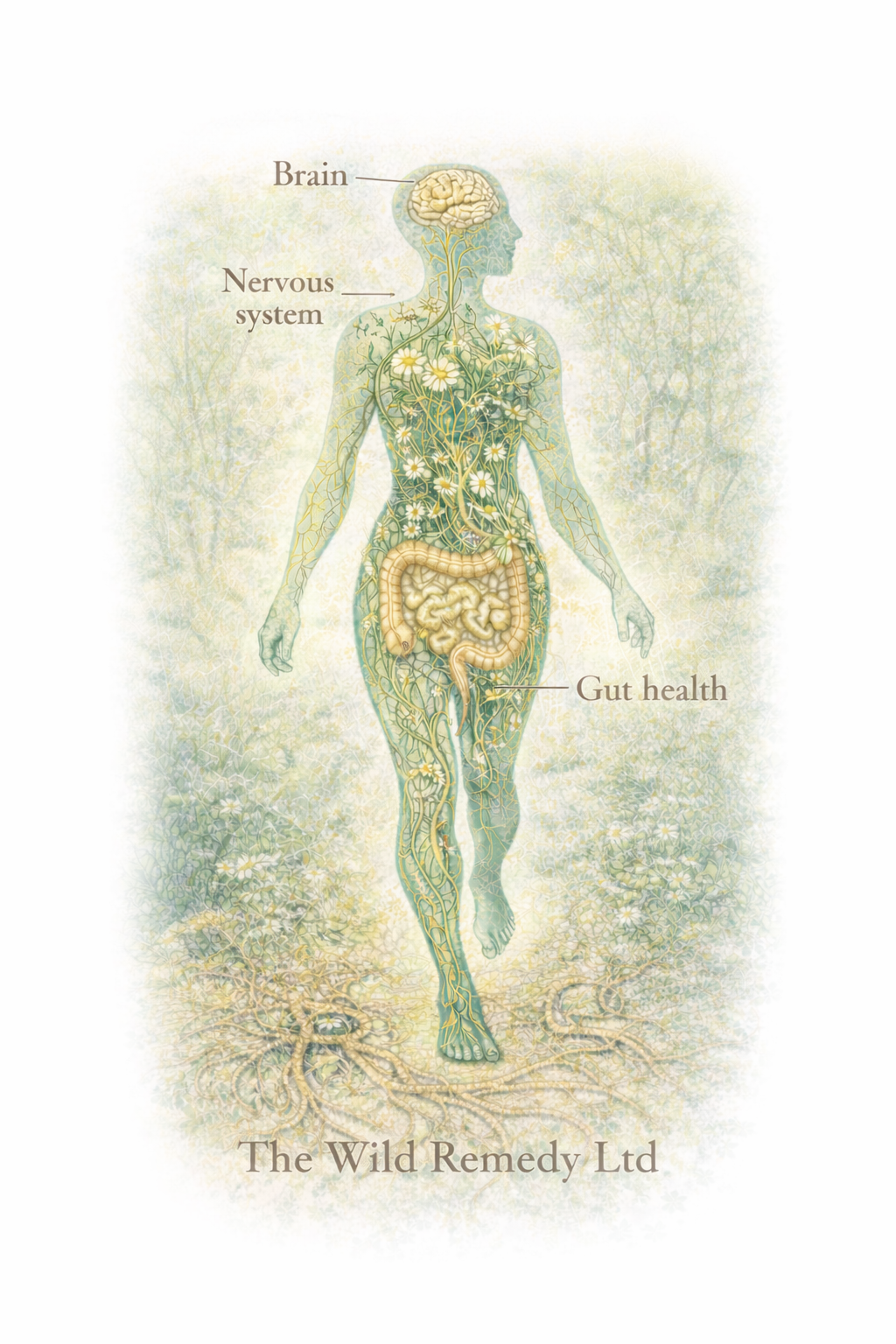
This is why it’s often called the second brain. Not because it thinks in words, but because it listens, signals, and remembers. It speaks to the nervous system, influences mood and motivation, and plays a role in how safe or unsettled we feel in ourselves. Much of our immune system is positioned here too — right where choice and protection meet.
So when we talk about caring for the gut, we’re not just talking about digestion. We’re talking about how we receive the world, how we respond to it, and how we restore ourselves when things fall out of balance.
What we begin with
One of the most grounding things I’ve been learning through my herbal medicine studies — including a focus on children’s herbal medicine — is how much of our gut and immune story begins before we ever make a conscious choice.
Long before birth, the body is already preparing.
While a baby develops in the womb, their immune system is being shaped by the mother — through her nutrition, her environment, her stress levels, and her own gut health. At birth, this process continues. The way a baby enters the world, the microbes they first encounter, and the early environment they are held in all help seed their developing gut flora.
Breastfeeding, where possible, plays a particularly important role. Breast milk doesn’t just provide nourishment — it contains immune factors and specific compounds that help feed beneficial bacteria in the baby’s gut, supporting both digestion and immune development. In this way, a mother’s nourishment becomes part of the child’s early microbiome story.
This doesn’t mean the body is fragile, or that everything has to be perfect.
Babies are not born empty or deficient. They arrive equipped with remarkable, built-in intelligence — an immune system designed to learn, adapt, and respond. The gut and immune system develop together, shaped by early inputs, but always with an underlying capacity for balance and resilience.
What early life shows us is not that health is fixed or predetermined, but that relationship matters. Nourishment, environment, rhythm, and care all influence how the system unfolds — and those influences continue throughout life.
In herbal medicine, especially when working with children, this understanding invites gentleness. Rather than trying to correct or control, we focus on supporting what is already there — trusting the body’s innate design while tending the conditions that allow it to flourish.
Why plant foods matter (without dogma)
There’s a growing conversation around plant-based eating, and it can quickly become polarised. My own view sits somewhere quieter.
Before the flood, the biblical narrative tells us humans ate plants — not as a rulebook, but as a picture of origin. Food as nourishment, medicine, and relationship. “I give you every seed-bearing plant…”
Modern research echoes this in its own language. Diverse plant fibres feed gut microbes. Polyphenols modulate inflammation. Bitter and aromatic compounds stimulate digestion. Whole plants bring complexity rather than single answers.
That doesn’t mean one way of eating fits everyone. Bodies are personal. Context matters. Culture matters. Season matters.
But it does suggest that our bodies recognise and respond to real food, grown from the earth, carrying information far beyond calories.
Movement: tending the garden through motion
If the gut is a garden, then movement is part of the tending.
Nothing in the body functions in isolation. Digestion does not happen on its own, and neither do immunity, mood, or resilience. The gut sits at the crossroads of these systems, and all of them depend on flow. When movement is absent, stagnation doesn’t announce itself loudly — it settles in quietly.
There is no pump for the lymphatic system (I will be taking you through the lymphatic system as part of this journey as we approach Spring). Digestion relies on rhythm. The nervous system responds to safety and ease. Even the microbial life within the gut responds to how we move — long periods of stillness alter diversity, signalling, and inflammatory tone.
This is where the idea of “fixing” one part of the body begins to fall apart.
We cannot restore homeostasis by focusing on food alone, or supplements alone, or exercise alone. The body always responds as a whole. What affects the gut affects the immune system. What affects the nervous system affects digestion. What affects movement affects everything.
Research now reflects this more clearly — showing that regular physical activity supports emotional wellbeing and resilience as effectively as many established approaches. But the deeper message isn’t about performance or prescription. It’s about participation.
As someone with a background in exercise science, I’ve seen how easily movement can become another place of pressure — targets, intensity, effort — and how easily that can disconnect people from their bodies rather than bring them back into relationship with them.
The body doesn’t respond only to optimal programmes — it responds to rhythm, consistency, enjoyment, and safety.
Walking. Gardening. Stretching. Dancing in the kitchen. Carrying shopping. Tending the soil.
The gut, the lymphatic system, and the nervous system all rely on movement. There is no pump for the lymphatic system. Digestion depends on flow. The nervous system settles when movement feels natural rather than forced.
Getting people moving in ways they enjoy and can sustain is far more powerful than prescribing perfection.
A gentle place to begin
And if all of this feels like a lot, there is comfort in starting small.
Just as we wouldn’t overhaul a garden overnight, the body responds best to simple, consistent acts of care. Often it’s not about doing more, but about doing less — and doing it with intention.
One of the gentlest ways to begin tending the gut is through a daily herbal infusion. Not as a fix or a cleanse, but as a quiet ritual — a moment of pause that supports both digestion and the nervous system.
A simple gut-soothing herbal tea
This blend is gentle, widely tolerated, and suitable for most people.
You’ll need:
Chamomile flowers
Lemon balm leaf
Freshly boiled water
A mug you enjoy using
How to prepare:
Add 1 teaspoon of chamomile and 1 teaspoon of lemon balm to your mug (you could use a muslin tea bag)
Pour over hot (not aggressively boiling) water
Cover and infuse for 8–10 minutes
Strain, sip slowly, and drink warm
This tea can be taken once daily, ideally at a quiet moment — after a meal, before bed, or whenever you feel the need to slow down.
If you want to learn more about growing & making your own herbal teas contact us to book one of our bespoke tea workshops.
Why this works:
Chamomile helps soften tension in the gut and nervous system
Lemon balm gently supports digestion while calming mental restlessness
Together, they encourage relaxation, rhythm, and ease — creating the conditions where balance can return
Other gentle ways to support the gut
In a world full of messages about detoxing, fasting, cleansing, and constant optimisation, it can be easy to forget that the body already has its own highly intelligent systems of balance and elimination.
Sometimes supporting the gut isn’t about doing more — it’s about stepping back.
A few simple, grounded places to begin:
Pause unnecessary supplements, especially synthetic ones taken “just in case” rather than for a clear reason. More isn’t always better, and layering products can sometimes overwhelm rather than support the gut ecosystem.
Eat simply for a few days, focusing on whole, familiar foods rather than restriction or extremes. Chewing more than feels necessary. Including bitter greens or herbs. Stability often does more for gut flora than constant dietary change.
Be cautious with harsh detoxes or prolonged fasting, which can strip beneficial bacteria and nutrients as easily as they remove what we don’t want.
Create regularity — eating at similar times, easting without rushing, sleeping consistently, and allowing the gut to settle into rhythm.
Let the body do what it’s designed to do, trusting that balance returns more easily when we stop fighting the system.
These are not rules or protocols — just gentle invitations to create the conditions where the gut can regulate itself again.
What we lost connection to
Somewhere along the way, we became disconnected from:
food as medicine,
movement as nourishment,
the body as intelligent,
and nature as teacher rather than backdrop.
We outsourced knowledge to labels, metrics, and experts, and forgot how to listen — inwardly and outwardly. The answers were always here: in plants, in seasons, in the way the body responds when we care for it gently.
Science isn’t contradicting this.
It’s catching up.
A living invitation
As we move towards February — a month we’ll be dedicating to the heart in all its emotional, physical, and relational meanings — it feels important to acknowledge that the gut and the heart are not separate stories. They are in constant conversation.
If this resonates, you’re warmly invited to:
book onto one of our nature-based workshops,
explore our handcrafted herbal products,
collaborate on therapeutic garden or wellbeing projects,
or join the Wild Circle, our slower, seasonal community space.
This is a journey — not a destination. One of reconnection, curiosity, and care.
💜
Further Reading
Books
Enders, G. (2016). Gut: The Inside Story of Our Body’s Most Underrated Organ. Scribe Publications.
A friendly, accessible, and often humorous introduction to the digestive system, the gut–brain connection, and emerging research around gut flora. An excellent starting point for readers new to the subject.
Blaser, M. J. (2014). Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues. Henry Holt and Company.
A detailed, well-referenced exploration of the human microbiome and the long-term consequences of antibiotic overuse on immune, metabolic, and inflammatory health.Ralph, J., & Tassell, M. (2021). Native Healers: Foundations in Western Herbal Medicine. Aeon Books.
The core accompanying text for Heartwood Education, offering a holistic framework for understanding human physiology, herbal therapeutics, and the interconnected nature of body systems.Waugh, A., & Grant, A. (2010). Ross and Wilson Anatomy and Physiology in Health and Illness (12th ed.). Churchill Livingstone.
A comprehensive anatomy and physiology reference, useful for grounding holistic health perspectives in structural and functional understanding.Waugh, A., & Grant, A. (2014). Ross and Wilson Anatomy and Physiology Colouring and Workbook (4th ed.). Churchill Livingstone.
A visual and practical companion to anatomy study, particularly helpful for embodied learning.Kapit, W., & Elson, L. (2013). The Anatomy Colouring Book. Pearson Education.
A visual learning resource supporting understanding of anatomical systems.Kapit, W. (1999). The Physiology Colouring Book. Benjamin Cummings.
A complementary guide focused on physiological processes.
Articles & Online Resources
The Brain–Gut–Microbiome Axis. National Center for Biotechnology Information (NCBI).
https://pmc.ncbi.nlm.nih.gov/articles/PMC6047317/The Gut–Brain Connection. Johns Hopkins Medicine.
https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-brain-gut-connectionDiet and the Microbiota–Gut–Brain Axis. NCBI Review.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8321864/